Trichuriasis (Whipworm) in Dogs
Both dogs and cats suffer from the whipworm
(Trichuris trichiura) parasite. It is generally transmitted by ingesting
infested matter, although whipworms can be contracted from other infected
animals. Whipworm eggs can live in an environment anywhere from a few months to
years, and can be present in soil, food, or water, as well as in feces or animal
flesh. Additionally, whipworms infect dogs of any
age.
Symptoms and Types
A whipworm infection may present itself as a large
bowel inflammation or bloody diarrhea, or it may be asymptomatic. Other symptoms commonly associated with a whipworm infection include dehydration,anemia, and
weight loss. It is worth noting that symptoms may begin prior to any visual
evidence of whipworm eggs.
Causes
Dogs contract whipworms by ingesting infested or
contaminated matter (e.g., food, water,
flesh).
Diagnosis
The veterinarian will confirm the diagnosis by
conducting the fecal flotation procedure on a stool sample. If parasitic eggs or
whipworms are present, they will float to the surface of the glass
slide.
Ancylostomiasis ( Hookworm) in Dogs
Hookworms can be fatal, especially in puppies. As
such, pet owners need to be vigilant for signs of hookworms in their dogs. These
blood-sucking parasites can invade, inhabit, and live in the dog's small
intestines. In their fourth-stage larvae, the hookworms can cause anemia and
inflammation in the dog's small intestine. Active worms leave bite sites and
those sites continue to seep blood.
Symptoms
A dog with the parasite looks unhealthy and has a poor
appetite; the linings of its nostrils, lips, and ears will be pale. If hookworm
larvae get into the lungs, the dog will cough, as well as present several other
symptoms, including dark and tarry stool, diarrhea, and constipation. Death can come suddenly if the dog is not immediatelytreated.
Causes
Puppies usually acquire this condition through
milk from their mothers. These infestations are always caused by ingestion or by
larval penetration of the skin, generally found in contaminated water or in a
contaminated environment.
Diagnosis
Hookworms cannot be seen with the naked eye and
must be therefore be microscopically examined by your veterinarian through a
stool specimen. This examination will also help the veterinarian determine what
course of treatment to prescribe. If some of the puppies in a litter have died,
hookworms should be suspected.
Cestodiasis ( Tapeworm ) in Dogs
Cestodiasis is the medical term for tapeworm
infestation. Tapeworms typically settle in the small intestine. The tapeworm
species can include Taenia, Dipylidium Caninum,
Echinococcus, and Mesocestoides. Treatment to destroy tapeworms is
critical to avoid transmission to humans (typically children) and to avert
damage to the dog's body. With prompt treatment, prognosis is
positive.
Symptoms
As the tapeworm grows, pieces of it break off
into segments and pass into the dog's intestines. You may see dried, white to
cream colored segments, or pieces, of tapeworm in the dog's feces or in the fur
under the tail. Some tapeworm species break off into segments that are too small
to see, while the segments of other tapeworm species will resemble sesame or
cucumber seeds in size and appearance. Still other species of worm will pass
into the feces and can be readily seen. Dogs may bite or lick the anus, or drag
their hind quarters across the floor in response to the
itching.
Causes
Tapeworms are acquired by ingesting the immediate
host containing larvae. Tapeworm eggs are frequently ingested through adult
fleas. Other sources that are potential transmitters, and that a dog is likely
to ingest, include rabbits, birds, and rodents. Scavenging may also lead to an
infestation of tapeworms.
Diagnosis
Tapeworms will be found in the anal sac or in the
feces of the animal. A fecal, or stool, sample can be used to review for the
presence of tapeworms. False negatives do occur, but most test results are
conclusive.
Ascariasis (Roundworms ) in Dogs
Is a disease affecting dogs caused by the
intestinal parasitic roundworm (or Ascaris lumbricoides). Roundworms are
often quite large -- up to 10 to 12 centimeters in length -- and can be present
in extremely high numbers within an infected animal. When they are found in a
dog's body, it can lead to abdominal swelling (distension), colic,
gastrointestinal issues and even intestinalrupture.
Symptoms
The following signs or symptoms are common in
dogs that have roundworms:
Colic - Lethargy - Vomiting - Abdominal - swelling -Abnormal feces - Poor nursing (in
females) - Anorexia -Coughing (caused when the roundworm larvae
have migrated into the dog's lungs)
Causes
Adult dogs can become infected through the
ingestion of roundworm eggs, which are found in infected food, water, vomit, or
feces. Pups can then contract the parasite during the pregnancy or by drinking
the milk from an infected pregnant animal. And if one of the newborns in a
litter is exposed to roundworms, the entire litter can contract the
parasite.
Diagnosis
Upon examination of the dog, a swollen abdominal
region is commonly detected. There may also be signs of weakness and loss of
appetite. A fecal swab will then be taken to detect the presence of roundworm
eggs. Dead roundworms being passed out of the animal's body is another good
indicator of the disease.
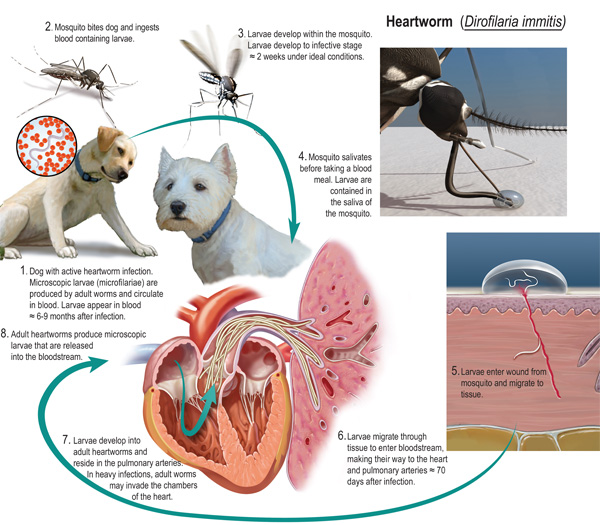
Dirofilariasis ( Heartworms ) in Dogs
Dogs suffering from heartworms are, in fact, infested by the organism Dirofilaria immitis, a parasitic nematode(roundworm) commonly referred to as the heartworm. The severity of this diseaseis directly dependent upon the number of worms present in the body, theduration of the infestation, and the response of the host (the infested dog is
the host).
In regions where Dirofilaria immitis isendemic, dogs without proper heartworm protection are almost 100 percent likelyto suffer from heartworm infestation. The heartworm is mainly endemic ingeographic areas with tropical and subtropical climates, and is also commonlyfound along the Atlantic and Gulf Coasts, and the Ohio and Mississippi river basins. The presence of Dirofilaria immitis is not limited to these areas, however, it is found worldwide. Dogs have been diagnosed with heartworm disease in all 50 U.S. states.
Heartworm disease is preventable with the administration of a heartworm prophylaxis (preventative) medication, as recommended by a veterinarian. For those dogs that do contract heartworm disease, the prognosis is good for mild to moderate cases, and such conditions can be relatively uneventful. Dogs with more severe cases may suffer from lung complications resulting from extreme medication given to kill serious infestations.
Symptoms and Types
Heartworm disease is defined in three classes, varying
in severity. Dogs with Class I heartworm disease are often asymptomatic, meaning
they exhibit no visible symptoms, or may only exhibit minimal signs such as an
occasional cough. Class II patients usually exhibit coughing and unusual
intolerance to exercise. The most severe cases, defined as Class III, may show
symptoms of anemia, exercise intolerance, fainting spells, and -- in
severely affected dogs, right-sided chronic heart failure.
A physical examination may reveal further symptoms,
especially in Class III cases. These include high blood pressure (hypertension), labored breathing, and extremely rapid heartbeat
(tachycardia).
Causes
Heartworms are spread through mosquitos that
carry the infective heartworm larvae. These larvae migrate from the bite wound
through the dog’s body until they reach the heart and blood vessels of the
lungs, a process that takes approximately six months. The larvae mature in the
dog’s body -- an adult heartworm can grow to be about 12 inches long. These adults reproduce and release immature heartworms, known as microfilariae,
directly into the dog’s blood. When a mosquito bites an already infected dog, it may take in these microfilariae with the dog’s blood, and then pass on the
infective heartworm larvae (the microfilariae develop once inside the mosquito)to another dog, thereby continuing the parasite’s life cycle and spreading the disease to the next host.
Risk factors associated with heartworm disease
include residence in endemic regions, such as tropical areas, outdoor habitation, and lack of the proper prophylaxis to prevent heartworm infestation.
Diagnosis
If heartworm disease is suspected, an electrocardiograph (which monitors changes in the heart) may reveal heart rhythm disturbances and/or enlargement of the right ventricle of the heart (hypertrophy).
Additional tests may include a urine analysis,
serologic tests that can identify the female heartworm antigen, and X-rays,
which may reveal enlargement in key arteries associated with heartworm disease.
Treatment
In initial treatment, most patients are hospitalized as they
receive administration of an adulticide designed to kill the adult heartworms.
The microfilariae in the body can be eliminated with a monthly prophylaxis,
which can be administered at home. For more severe cases, such as dogs
experiencing thromboembolic complications (in which a blood clot that has formed
breaks loose and travels through the blood stream to clot another vessel),
hospitalization may be necessary for a longer period of time.
In some cases, a surgical procedure may be necessary to remove
adult worms from the right heart and pulmonary artery by way of the jugular
vein. This procedure is recommended if the infestation consists of a high number
of adult worms.
Living and Management
Upon initial heartworm treatment, activity should be severely
restricted for at least four to six weeks after administration of the
adulticide. Severely affected dogs may need to be kept in a cage to limit
activity. For dogs recovering from congestive heart failure, a moderately
restrictive sodium diet is recommended.
An antigen test should be done four months after adulticide
treatment to check for continued presence of the adult Dirofilaria
immitis. If the test is positive, the adulticide treatment can be repeated,
or a surgical procedure performed instead. Some dogs with persistent infestation
may not require retreatment, depending on the patient’s age and severity of the
disease. Older dogs, for example, may not be overly affected by mild recurrent
worm infestations.
Prevention
Routine heartworm prophylaxis (preventative) should be given to
any at-risk dogs, for example those living in endemic regions, as directed by
your veterinarian. This is essential to preventing heartworm infestation. There
are a number of medical preventatives that are highly effective and commonly
used. It is possible for infestation to occur if a prophylaxis is not regularly
administered.
In initial treatment, most patients are hospitalized as they
receive administration of an adulticide designed to kill the adult heartworms.
The microfilariae in the body can be eliminated with a monthly prophylaxis,
which can be administered at home. For more severe cases, such as dogs
experiencing thromboembolic complications (in which a blood clot that has formed
breaks loose and travels through the blood stream to clot another vessel),
hospitalization may be necessary for a longer period of time.
In some cases, a surgical procedure may be necessary to remove
adult worms from the right heart and pulmonary artery by way of the jugular
vein. This procedure is recommended if the infestation consists of a high number
of adult worms.
Living and Management
Upon initial heartworm treatment, activity should be severely
restricted for at least four to six weeks after administration of the
adulticide. Severely affected dogs may need to be kept in a cage to limit
activity. For dogs recovering from congestive heart failure, a moderately
restrictive sodium diet is recommended.
An antigen test should be done four months after adulticide
treatment to check for continued presence of the adult Dirofilaria
immitis. If the test is positive, the adulticide treatment can be repeated,
or a surgical procedure performed instead. Some dogs with persistent infestation
may not require retreatment, depending on the patient’s age and severity of the
disease. Older dogs, for example, may not be overly affected by mild recurrent
worm infestations.
Prevention
Routine heartworm prophylaxis (preventative) should be given to
any at-risk dogs, for example those living in endemic regions, as directed by
your veterinarian. This is essential to preventing heartworm infestation. There
are a number of medical preventatives that are highly effective and commonly
used. It is possible for infestation to occur if a prophylaxis is not regularly
administered.
Coccidiosis in Dogs
Coccidiosis is a parasitic type of infection, caused by the
coccidian that most commonly causes watery, mucus-based diarrhea in dogs. If it
is not treated, over time it can cause damage to the lining of the dog's
intestinal tract. With treatment, the prognosis is
good.
Coccidia are parasites that are often misunderstood in dogs. After the first exposure, coccidia parasites are always present in the puppy’s intestines, and they’re just waiting to take advantage of any digestive upset. It is rarely the initial cause of the diarrhea, but once diarrhea starts, the coccidia will overgrow to large numbers to keep the diarrhea going.
Coccidia are a major issue for puppies under 8 weeks old.
Acquiring Coccidia
Puppies are born with a sterile gut, and their mother seeds their gut with good bacteria during cleaning them and caring for them. However, puppies can also get coccidia from their moms, so the goal is to keep the puppy’s exposure to a minimum number. There are a variety of products you can use for both treatment and prevention, but prevention is most important for consistently healthy puppies.
Symptoms and Types
You may notice that the dog has watery, mucous-like diarrhea. As
the condition progresses, bloody diarrhea and an inability to withhold it will
begin to show. The dog may also be in a weakened
state.
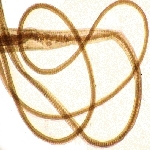
WHERE DO COCCIDIA COME FROM?
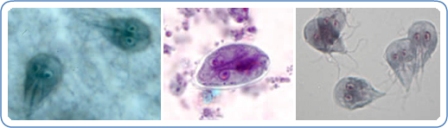
Oocysts (pronounced o'o-sists), like those shown above, are passed in stool.
In the outside world, the oocysts begin to mature or sporulate. After they have
adequately matured, they become infective to any host (dog or cat) that
accidentally swallows them.
To be more precise, coccidia come from fecal-contaminated ground. They are
swallowed when a pet grooms/licks the dirt off itself. In some cases,
sporulated oocysts are swallowed by mice and the host is infected when it eats
the mouse. Coccidia infection is especially common in young animals housed in
groups (in shelters, rescue areas, kennels, etc.) This is a common parasite and
is not necessarily a sign of poor husbandry.
WHAT HAPPENS INSIDE THE HOST?
The sporulated oocyst breaks open and releases eight sporozoites. These
sporozoites each finds an intestinal cell and begins to reproduce inside it.
Ultimately, the cell is so full of what are at this stage called merozoites
that it bursts, releasing the merozoites that seek out their own intestinal
cells and the process begins again. It is important to note how thousands of
intestinal cells can become infected and destroyed as a result of accidentally
swallowing a single oocyst.
As the intestinal cells are destroyed in larger and larger numbers,
intestinal function is disrupted and a bloody, watery diarrhea results. The
fluid loss can be dangerously dehydrating to a young or small pet.
HOW ARE COCCIDIA DETECTED?
A routine fecal test is a good idea for any new puppy or kitten whether there
are signs of diarrhea or not as youngsters are commonly parasitized. This sort
of test is also a good idea for any patient with diarrhea and is recommended at
least once a year for healthy dogs and cats as a screening test. The below
photograph shows coccidia oocysts seen under the microscope in a fecal sample.
Coccidia are microscopic and a test such as this is necessary to rule them in.
It should be noted that small numbers of coccidia can be hard to detect so just
because a fecal sample tests negative, this does not mean that the pet is not
infected. Sometimes several fecal tests are performed, especially in a young
pet with a refractory diarrhea; parasites may not be evident until later in the
course of the condition.
HOW IS COCCIDIA TREATED?
The most common medicines used against coccidia are called coccidiostats.
They inhibit coccidial reproduction. Once the numbers stop expanding, it is
easier for the patient’s immune system to catch up and wipe the infection out.
This also means, though, that the time it takes to clear the infection depends
on how many coccidia organisms there are to start with and how strong the
patient’s immune system is. A typical treatment course lasts about a week or
two, but it is important to realize that the medication should be given until
the diarrhea resolves plus an extra couple of days. Medication should be given
for at least 5 days total. Sometimes courses as long as a month are needed. In
dogs and cats, sulfa-based antibiotics are the most commonly used
coccidiostats.
The use of sulfa drugs in pregnancy can cause birth defects. Sulfa drug use
can also lead to false positive test results for urine glucose.
There is another medication that is worth mentioning and that is Ponazuril, a large animal
product. This medication is actually able to curtail a coccidial infection in
five doses or less and has been used in thousands of shelter puppies and
kittens with no adverse effects. This product would seem to be superior to the
usual sulfa drugs, but the problem that keeps it from becoming a mainstream
treatment is the fact that it is available only as a paste for horses and must
be diluted down to create an appropriate small animal formula. The large
volumes of product yielded are not cost effective if only occasional patients
are treated for this parasite. Ponazuril is thus most commonly used in kennels,
catteries, and animal shelters though one may be pleasantly surprised to find
it in stock at one's regular veterinary office.
CAN PEOPLE OR OTHER PETS BECOME INFECTED?
While there are species of coccidia that can infect people (Toxoplasma and Cryptosporidium,
for example), the Isospora species of dogs and cats are not infective to
people. Other pets may become infected from exposure to infected fecal matter
but it is important to note that this is usually an infection of the young
(i.e. the immature immune system tends to let the coccidia infection reach
large numbers whereas the mature immune system probably will not.) In most
cases, the infected new puppy or kitten does not infect the resident adult
animal.
Guide to Giardia in Dogs: Diagnosis, Treatment and
Prevention
Giardia in dogs (also known as giardiasis) became well known
several decades ago when a different strain of the organism was identified as
causing persistent diarrhea in people. Once an understanding was developed that
the condition is spread through feces contaminated swimming pools, food,
drinking water, and surfaces, did the awareness of the disease increase. This
awareness led to an understanding of giardiasis in animal health and
improvements in detection methods.
Causes of Giardia in Dogs (Left and right: Giardia Protozoa ;
Center: Cyst) Source: CDC
Studies show that approximately 4% to 6.8% of dogs shed giardia
cysts. The cysts are shed by infected dogs from the small intestines and are
passed through the feces. Rates of infection are higher in younger dogs with 12%
of dogs under age 6 months testing positive for the disease. This rate is
significantly lower in dogs 3 and older, where only 1%$ shed
cysts.
The protozoa that causes giardia in
dogs are transported in protective cysts
which protect the protozoa until they reach the next host. Giardia can last in
the environment for several months.
How Giardiasis is Spread from Dog to Dog
The infection spreads when a dog ingests cysts found in feces
after ingesting contaminated water, food, or from fomites in the environment
such as a park, improperly cleaned kennel or dog run. Once the cysts are
ingested, the giardia protozoa begin to multiply and attach to the dog’s small
intestine. As they feed off the dog, they rob the dog of nutrients through
mal-absorption and problems with the digestive system through mal-digestion
(incomplete digestion). Protozoa that feed on a host are referred to as
trophozoites. Any surface that is contaminated, including food, play toys etc
that came in contact with feces from a dog that is shedding giardia cysts, can
be one of thecauses of giardia in dogs.
A dog will start shedding cysts in 5 to 7 days after being
infected.
Each Person, Dog or Cat is infected with a different strain of
Giardia
The giardia that infects dogs (giardia canis) is different than
the giardia that infects cats (giardia felis) or the strain seen in humans. In
general, dogs in the Northeastern United States have a higher incidence of the
disease over the Southeastern United States (DD Bowman 2011, Carlin
2006).
Dog Giardia Symptoms
The most common giardia dog symptoms are moderate to severe
diarrhea with or without mucus. It is rare for the diarrhea to contain blood.
Other symptoms includes vomiting. Most dogs that shed giardia cysts are
asymptomatic, which means that they do not show any giardia
symptoms.
Diagnosis of Dog Giardia
Giardia diiagnosis in dogs is accomplished in the veterinarian’s office with one of several types of tests. This includes a centrifugal fecal flotation test or fecal ELISA test. Note that the majority of dogs are asymptomatic or symptom free. In this case, giardia in
dogs is detected as part of tests conducted during a checkup, called fecal
centrifugation. If this is the case, your veterinarian will discuss with you the
pro’s and cons of treating a dog that does not show symptoms.
Canine Giardia Treatment
There are several prescription medications available for
giardia dog treatment.
This includes:
Fenbendazole/febantel (50 mg/kg for 5 days) is effective in
most dogs.
- Metronidazole (25 mg/kg 5 days). In some dogs Metronidazole
can be toxic (Per 2010 CAPC Guidelines).
Drontal Plus (3 days)
Homeopathic supplements can help to restore digestive health
after prescription treatment.
If a dog becomes severely dehydrated from the diarrhea, fluid
therapy in the veterinarian’s office will be
necessary.
Dog Giarda Vaccine
The dog giardia vaccine is not considered a core or mandatory
vaccine. Exposure of a dog to potential sources of giardia such as other dogs
and contaminated waterways should be considered as part of the decision to
vaccinate.
Can Humans Catch Giardia from Dogs (Zoonotic)?
The strain of giardia found in humans has been found as the
source of infection in a limited number of dog giardia cases. For this reason,
there is some risk that giardia can pass from human to dog. If a dog is infected
with a human strain it could theoretically pass back to humans, although this is
considered to be rare. Because of this, proper hygiene should be followed when
handling an infected dog. Always be careful when disposing of
feces.
Giardia Dog Prevention
Only give your dog fresh drinking water when outdoors. Avoid
allowing your dog to drink from any standing water that could be contaminated.
If your dog defecates outdoors, such as in a backyard, clean-up all feces. Dogs
that have been positively diagnosed should have a bath to remove any cysts that
could be hiding in the coat.
These hygienic steps are necessary to prevent reinfection, as it
is common for this to occur in giardia in dogs
cases.
can be toxic (Per 2010 CAPC Guidelines).
Drontal Plus (3 days)